You can listen to an audio version of this newsletter above. Please note that this is unedited and there may be some natural stumbles, as I’m recording in my home office.
New Podcast + Video Interview!
Dr. Talia Jackson and Doug Jensen invited me to talk about Slow Productivity and so much more on their show “We’re Not Fine.” You can listen to the episode here in audio format or you can click here or below to watch our conversation as a video.
I hope you enjoy listening as much as I enjoyed chatting with Dr. Talia and Doug!
The concept for this letter originated on a recent coaching call with a client who just completed their first semester as a tenure-track professor.
We were discussing the challenge of stopping yourself from doing extra work—especially when getting a bit ahead at work means having less energy to cook, tend to your home, and do self-care practices. It’s a complex topic, so I’m going to explore it today through the lens of fatigue and chronic illness. But even if you don’t live with a chronic health condition, I hope these musings on energy encourage some self-reflection.
What’s Energy?
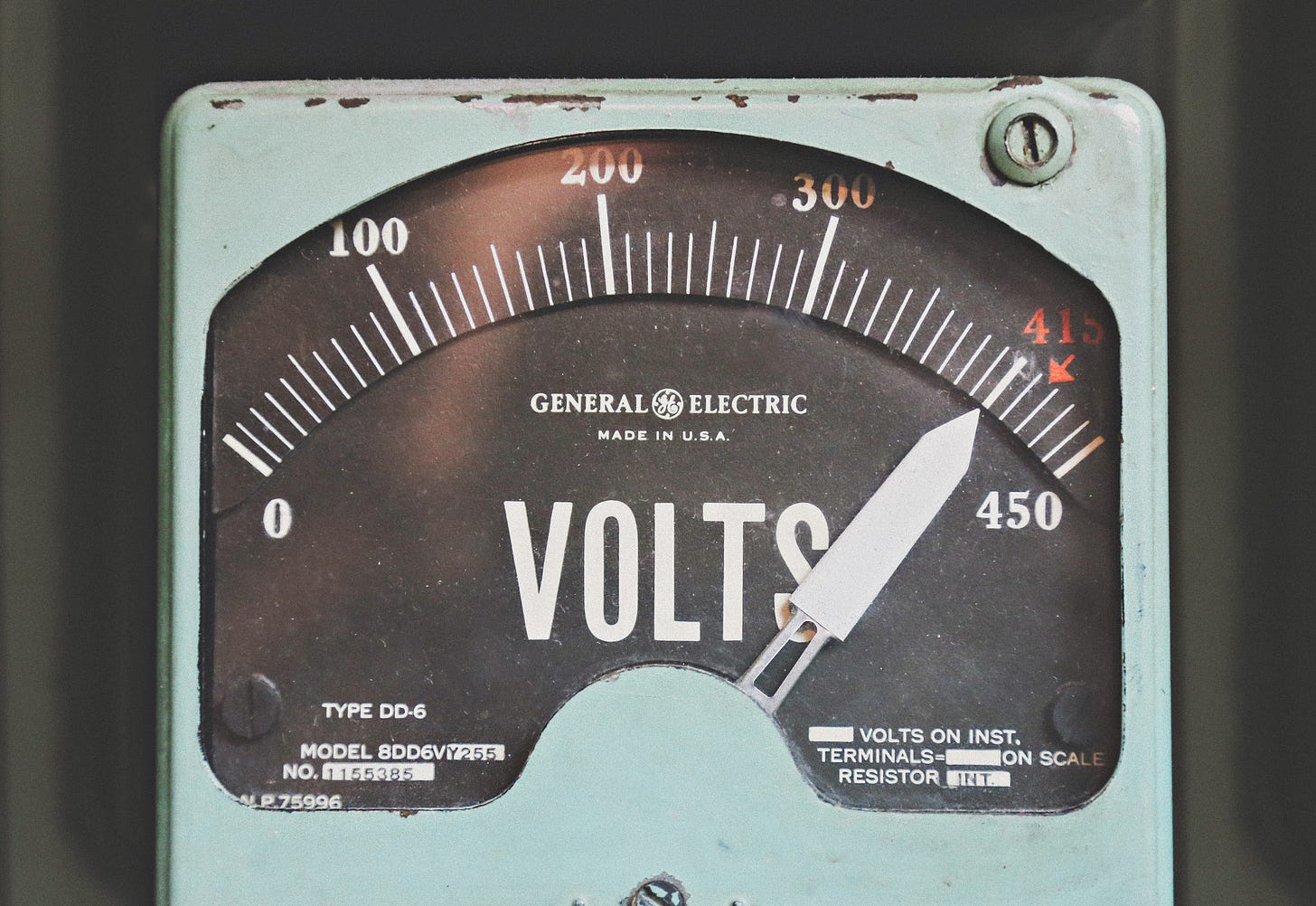
When I think of energy, my first thought is the invisible spark in our walls that keeps our refrigerators cold and our lamps bright. For most of us, this energy comes from a local electric company, and if you live in a place like I do that gets cold in the winter, those bills can get very high.
I know I may sound cynical for jumping right to transactions, but energy exchange is something I think a lot about as a chronically ill person. Not in terms of the number on my thermostat, but in what will it cost me—physically, emotionally, mentally—to complete the tasks on my to-do list.
Some of us are able to top off our internal batteries by sleeping a few extra hours or drinking an afternoon coffee—but that experience is not the norm. Our physical, mental, and emotional energy is a precious resource that may ebb or flow in ways we can’t always predict, so it makes complete sense that we might choose to exert ourselves when we do have energy to spare.
Spoon Theory & Fatigue
Spoon Theory can be helpful here. Created by Christine Miserandino, Spoon Theory is a metaphor used to explain the daily experience of having chronic illness to someone who does not share the same experience (here’s Miserandino’s PDF of the Spoon Theory). By giving her “healthy” friend 12 spoons and taking away spoons to represent energy expenditure on tasks such as preparing for work, traveling, cooking, and dealing with emergencies, Miserandino “explained that the difference in being sick and being healthy is having to make choices or to consciously think about things when the rest of the world doesn’t have to.” The Spoon Theory thus serves as a metaphor to show that people expend energy differently.
If you do live with a chronic illness, learning how to assess your spoon levels or estimate how many spoons you have on particular days is a helpful tool. But your to-do list persists, regardless of your spoon count. For example, when I have a flare-up of my chronic illness, the effort to hold my arms up and wash my hair can exhaust me. So, I have to intentionally choose between washing my hair or completing a to-do list item that feels more urgent, because I simply don’t have enough spoons to do both.
I’m not alone in this feeling of fatigue. While my fatigue is a symptom of my two chronic health conditions, it is also incredibly common for folks who live with conditions like Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and Long Covid.
According to a 2015 report from the Institute of Medicine, 836,000 to 2.5 million Americans have ME/CFS. A December 2023 report from the National Center for Health Statistics reported that 1.3% of adults had ME/CFS in 2021-2022 (this number might actually be an underrepresentation, though, because survey respondents were asked if they had been officially diagnosed by a doctor with ME/CFS, and the CDC reports that ME/CFS is challenging to diagnose).
A 2023 article in Nature suggests that at least 65 million people have Long Covid worldwide, though that number is also believed to be quite conservative. Long Covid is different for everyone who has it, but symptoms include fatigue and ongoing difficulty with breathing, concentration, digestion, and more.
The Energy Trade-off
People with ME/CFS, Long Covid, and other chronic health conditions experience post-exertional malaise, where physical and mental activities result in increased symptoms that may last for long durations of time.
I bring this up because sometimes draining your energy levels looks less like “going above and beyond” (i.e., pulling an all-nighter, running a marathon, cleaning your whole house in one day) and more like triaging your energy in order to meet your basic needs.
Today I’ve focused a lot on the ways chronically ill folks experience energy expenditure, but by no means are we the only people who are forced to make the unfair decision between working and caring for ourselves. I recommend Dr. Devon Price’s Substack letter “Work is a Chronic Illness” as an example of interrogating our acceptance of a 40-hour workweek (and in some places, way more than 40) when overwork can traumatize and exhaust our bodies, brains, and spirits.
Should You Work Ahead?
I’m intentionally choosing not to leave you with a go-to formula or a “best practices” approach for managing your own energy levels. That being said, I do hope that you’ll pause the next time you think “huh, should I rest or work ahead?” if you’re faced with time and energy to spend as you wish.
I’d love to hear your reflections and thoughts on today’s letter, including resources you think are helpful around this topic.
Further Reading & Resources
KC Davis’s book How to Keep House While Drowning offers a compassionate and actionable approach to caring for your foundational needs at home when you have limited energy.
I’ve found Jace Harr’s “You Feel Like Shit: An Interactive Self-Care Guide” and Sinope’s “Everything is Awful and I’m Not Okay: Questions to Ask Before Giving Up” to be very helpful for days when it’s hard to identify which eating/drinking/resting/hygiene actions are truly necessary and most accessible.
I’ll be back next week with a Curiosities post about one of my favorite genres. In the meantime, I invite you to please submit a question for the January Q&A post, which is now free for all subscribers.
Take care and talk soon,
Dr. Kate